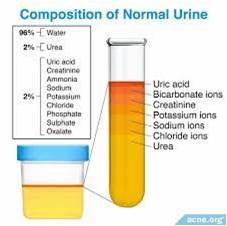
Microscopic Examination of Urine: Microscopic examination of urine, also known as a urine sediment analysis, is a laboratory test that involves the examination of a small sample of urine under a microscope. This test is often performed as part of a urinalysis, which is a routine screening test used to assess overall kidney and urinary tract health, as well as to help diagnose various medical conditions.
The Microscopic Examination of Urine
Microscopic examination of urine is a laboratory test that analyzes a small sample of urine under a microscope to evaluate the physical, chemical, and microscopic characteristics of the urine. It helps to diagnose various health conditions, such as urinary tract infections, kidney disease, and bladder cancer. Some of the main aspects of microscopic examination of urine are:
Sample collection and preservation: A mid-stream, freshly voided, first morning specimen is preferred since it is the most concentrated. The specimen should be examined within 2 hours of voiding because cells and casts degenerate upon standing at room temperature. If preservative is required, then 1 crystal of thymol or 1 drop of formalin (40%) is added to about 10 ml of urine.
Method of examination: A well-mixed sample of urine (12 ml) is centrifuged in a centrifuge tube for 5 minutes at 1500 rpm and supernatant is poured off. The tube is tapped at the bottom to resuspend the sediment (in 0.5 ml of urine). A drop of this is placed on a glass slide and covered with a cover slip. The slide is examined immediately under the microscope using first the low power and then the high power objective.
Microscopic Examination of Urine: A trained laboratory technician or pathologist examines the sediment portion of the urine under a microscope. They typically look for various types of norml and abnorml findings in the urine. ‘Microscopic Examination of Urine’
Normal and abnormal findings: Normally, there is no sediment or very little. The following table shows the normal contents of the sediments:
| Normal contents of the urine | Findings in the normal sediments |
|---|---|
| White blood cells | Variable in males and females. Maybe 0 to 5 /HPF |
| Red blood cells | Variable and maybe 0 to 2 /HPF |
| Epithelial cells | Variable in males and females but more in females 1 to 5 /HPF |
| Bacteria | Negative |
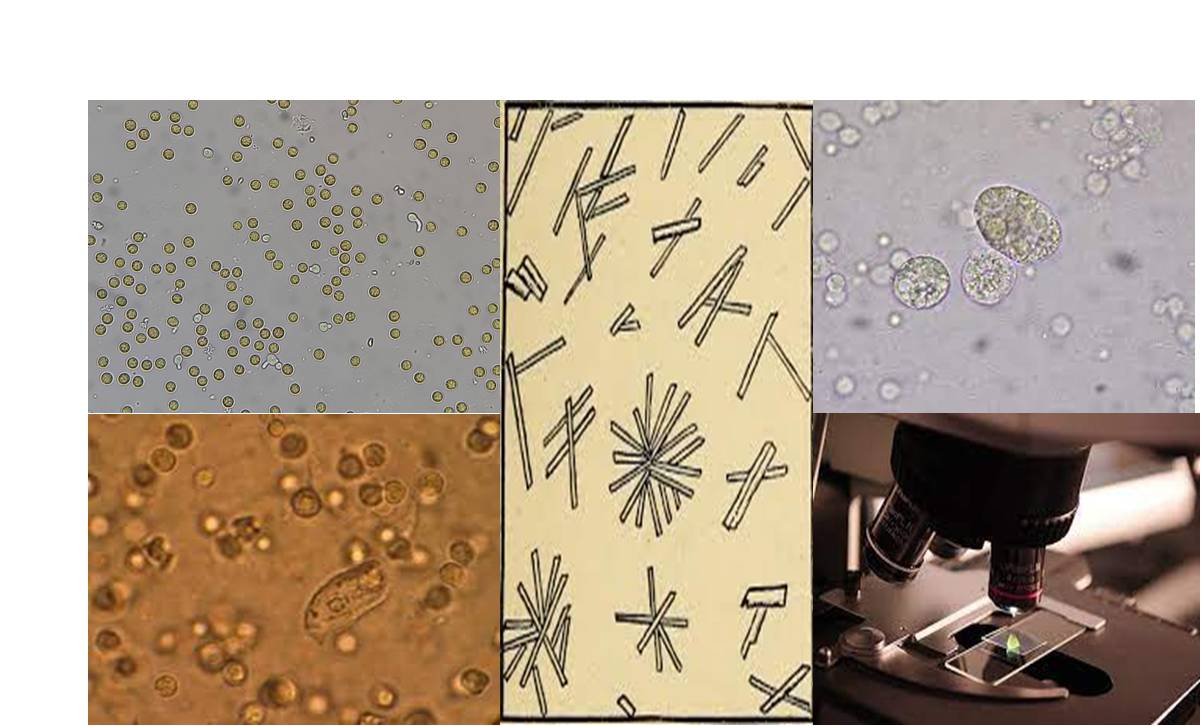
Abnormal findings include various types of cells, casts, crystals, bacteria, yeast, parasites, and other substances that indicate inflammation, infection, damage, or disease of the urinary tract. Some examples are:
Red blood cells: Hematuria (presence of blood in urine) can be caused by glomerulonephritis, kidney stones, urinary tract infections, tumors, trauma, or anticoagulant therapy. Dysmorphic red blood cells (abnormally shaped) are suggestive of glomerular origin of hematuria.
White blood cells: Pyuria (presence of pus in urine) can be caused by urinary tract infections, interstitial nephritis, glomerulonephritis, or tuberculosis. Eosinophils (a type of white blood cells) can be seen in allergic interstitial nephritis, a drug-induced kidney disorder.
Epithelial cells: Squamous epithelial cells are derived from the lower urinary tract and are usually insignificant. Clue cells are squamous epithelial cells covered with bacteria and indicate bacterial vaginosis. Transitional epithelial cells are derived from the renal pelvis, ureter, bladder, or urethra and can be seen in increased numbers in urinary tract infections, catheterization, or tumors. Renal tubular epithelial cells are derived from the kidney tubules and indicate tubular necrosis, viral infections, or rejection of a transplanted kidney.
Fat globules and fat bodies: Fat globules are free-floating lipid droplets that can be seen in nephrotic syndrome, a condition characterized by proteinuria, hypoalbuminemia, and edema. Fat bodies are renal tubular epithelial cells or casts that contain fat globules. They can be identified by their refractile appearance and Maltese cross pattern under polarized light.
Bacteria: Bacteria can be seen in urine as single cells, pairs, chains, or clusters. They indicate a urinary tract infection, especially if accompanied by white blood cells and positive nitrite and leukocyte esterase tests. Some bacteria can also cause urine to become alkaline and produce ammonia, which can lead to the formation of crystals and stones.
Yeast: Yeast are oval or round cells that can be seen in urine as budding forms or pseudohyphae. They indicate a fungal infection of the urinary tract, which can occur in diabetic patients, immunocompromised patients, or patients on antibiotic therapy. Candida albicans is the most common cause of urinary yeast infection.
Trichomonas: Trichomonas are flagellated protozoa that can be seen in urine as motile cells with undulating membranes. They indicate a parasitic infection of the urinary tract, which is sexually transmitted. Trichomonas vaginalis is the most common cause of urinary trichomoniasis.
Casts: Casts are cylindrical structures that are formed in the kidney tubules and have the same diameter as the tubules. They consist of a protein matrix and may contain cellular or non-cellular elements. The type and number of casts can provide information about the location and severity of kidney damage. Some common types of casts are:
- Hyaline casts: Hyaline casts are composed of only protein and have a clear, transparent appearance. They are the most common type of casts and can be seen in normal or concentrated urine, or in conditions such as fever, exercise, or diuretic therapy.
- Granular casts: Granular casts are composed of protein and granules that are derived from the breakdown of cellular casts or the inclusion of cellular debris. They have a coarse, granular appearance and can be seen in conditions such as acute tubular necrosis, glomerulonephritis, or pyelonephritis.
- Waxy casts: Waxy casts are composed of protein and have a smooth, waxy appearance and brittle consistency. They are formed from the degeneration of granular casts and indicate chronic renal failure.
- Fatty casts: Fatty casts are composed of protein and fat globules that are derived from the breakdown of fat bodies. They have a highly refractile appearance and can be seen in nephrotic syndrome.
- Red blood cell casts: Red blood cell casts are composed of protein and red blood cells. They have a yellowish-brown or orange color and indicate glomerulonephritis, vasculitis, or malignant hypertension.
- White blood cell casts: White blood cell casts are composed of protein and white blood cells. They have a grayish-white or yellowish color and indicate pyelonephritis, interstitial nephritis, or acute glomerulonephritis.
- Tubular cell casts: Tubular cell casts are composed of protein and renal tubular epithelial cells. They indicate tubular damage or necrosis, which can be caused by various conditions such as acute tubular necrosis, viral infections, or transplant rejection.
Crystals: Crystals are formed from the precipitation of solutes in urine. They can have various shapes, sizes, and colors depending on the type of solute and the pH and concentration of urine. Some crystals have little clinical significance, while others indicate metabolic disorders or urinary tract infections. ‘Microscopic Examination of Urine consisting some common types of crystals are:
- Calcium oxalate crystals: Calcium oxalate crystals are derived from oxalic acid and calcium. They can have various shapes, such as octahedrons (envelopes), dumbbells, or ovals. They can be seen in normal urine, or in conditions such as ethylene glycol poisoning, renal tubular acidosis, or oxalate stones.
- Triple phosphate crystals: Triple phosphate crystals are derived from ammonium, magnesium, and phosphate. They have a coffin-lid or prism shape and are also known as struvite crystals. They can be seen in alkaline or infected urine, or in conditions such as struvite stones or urea-splitting bacterial infections.
- Uric acid crystals: Uric acid crystals are derived from uric acid, a product of purine metabolism. They can have various shapes, such as rhomboids, rosettes, or needles. They can be seen in acidic or concentrated urine, or in conditions such as gout, leukemia, or uric acid stones.
- Cystine crystals: Cystine crystals are derived from cystine, an amino acid. They have a hexagonal shape and are colorless and transparent. They can be seen in acidic or neutral urine, or in conditions such as cystinuria, a genetic disorder of amino acid transport, or cystine stones.
- Tyrosine crystals: Tyrosine crystals are derived from tyrosine, an amino acid. They have a fine needle shape and are yellow or brown. They can be seen in acidic or neutral urine, or in conditions such as liver disease or tyrosinemia, a genetic disorder of tyrosine metabolism ‘Microscopic Examination of Urine’
Preparation of Urine Report
The results of a microscopic examination are usually reported along with other findings from a urinalysis, such as the color, clarity, pH, and specific gravity of the urine. These results, along with the patient’s medical history and clinical symptoms, help healthcare providers make a diagnosis or further investigate any underlying health issues. It’s important to note that a urine sediment analysis is just one part of the diagnostic process, and additional tests may be required to confirm or further evaluate any abnormalities found during the microscopic examination of urine. ‘Microscopic Examination of Urine’
Preparing a urine report involves documenting the findings from various urine tests, including a physical examination, chemical analysis, and microscopic examination of the urine sample. Here is a step-by-step guide on how to prepare a urine report:
Patient Information: Begin by including essential patient information, such as the patient’s name, date of birth, gender, and any relevant medical identification numbers or codes.
Date and Time of Sample Collection: Clearly state the date and time when the urine sample was collected. This information is crucial for tracking changes over time. ‘Microscopic Examination of Urine’
Sample Collection Details: Document how the urine sample was collected, including whether it was a random sample, midstream catch, or from a catheter. Note any relevant details, such as the patient’s fasting status or recent medications. “Microscopic Examination of Urine”
Physical Examination:
- Color: Describe the color of the urine sample, which can range from pale yellow to dark amber. Use descriptive terms like “straw-yellow,” “amber,” “cloudy,” or “bloody” if applicable.
- Clarity: Mention the clarity of the urine, which can be clear, slightly cloudy, or cloudy. Note if it appears turbid due to the presence of particles or sediment. ‘Microscopic Examination of Urine’
- Odor: Describe the odor of the urine, which can vary from mild to strong. Common descriptors include “ammonia-like,” “sweet,” “foul,” or “normal.”
Chemical Analysis: Include the results of the chemical analysis, which typically includes the following parameters:
- pH Level: Report the pH level of the urine, which indicates its acidity or alkalinity.
- Specific Gravity: Mention the specific gravity of the urine, which reflects the concentration of solutes in the urine.
- Protein: Indicate whether protein is present in the urine and note the amount if it’s above the normal reference range. ‘Microscopic Examination of Urine’
- Glucose: Report the presence or absence of glucose in the urine.
- Ketones: Note the presence or absence of ketones in the urine.
- Bilirubin: Indicate whether bilirubin is present in the urine.
- Blood: Report the presence of blood in the urine and note whether it is hemoglobin (hematuria) or red blood cells (hematuria or hemoglobinuria). ‘Microscopic Examination of Urine’
- Leukocytes: Mention the presence of leukocytes, which can indicate infection or inflammation.
Microscopic Examination of urine: Describe the findings from the microscopic examination of the urine sediment. This may include:
- Red Blood Cells (RBCs): Report the presence and quantity of RBCs.
- White Blood Cells (WBCs): Report the presence and quantity of WBCs.
- Epithelial Cells: Mention the type and quantity of epithelial cells observed.
- Crystals: Describe any crystals seen and their types. ‘Microscopic Examination of Urine’
- Casts: Report the presence and type of casts. ‘Microscopic Examination of Urine’
- Bacteria and Yeast: Indicate if bacteria or yeast are present.
- Other Particles: Mention any other notable findings, such as mucus or parasites.
Interpretation: Provide an interpretation of the findings, explaining what the results suggest in the context of the patient’s clinical condition. If any abnormalities are detected, mention possible causes or conditions that may need further investigation. ‘Microscopic Examination of Urine’
Laboratory Information: Include the name and contact information of the laboratory where the analysis was performed. Also, include the names and signatures of the healthcare professionals who conducted and reviewed the test results. ‘Microscopic Examination of Urine’
Reference Ranges: Include reference ranges for each parameter to help clinicians assess whether the results fall within normal limits.
Attachments: If applicable, attach any images or photomicrographs of the urine sediment to support the findings.
Additional Notes: Include any additional notes or observations that may be relevant to the interpretation of the results. ‘Microscopic Examination of Urine’
Remember that the format and specific details included in a urine report may vary depending on the laboratory’s protocols and the healthcare facility’s requirements. It’s essential to follow the established guidelines and standards for reporting urine test results accurately.